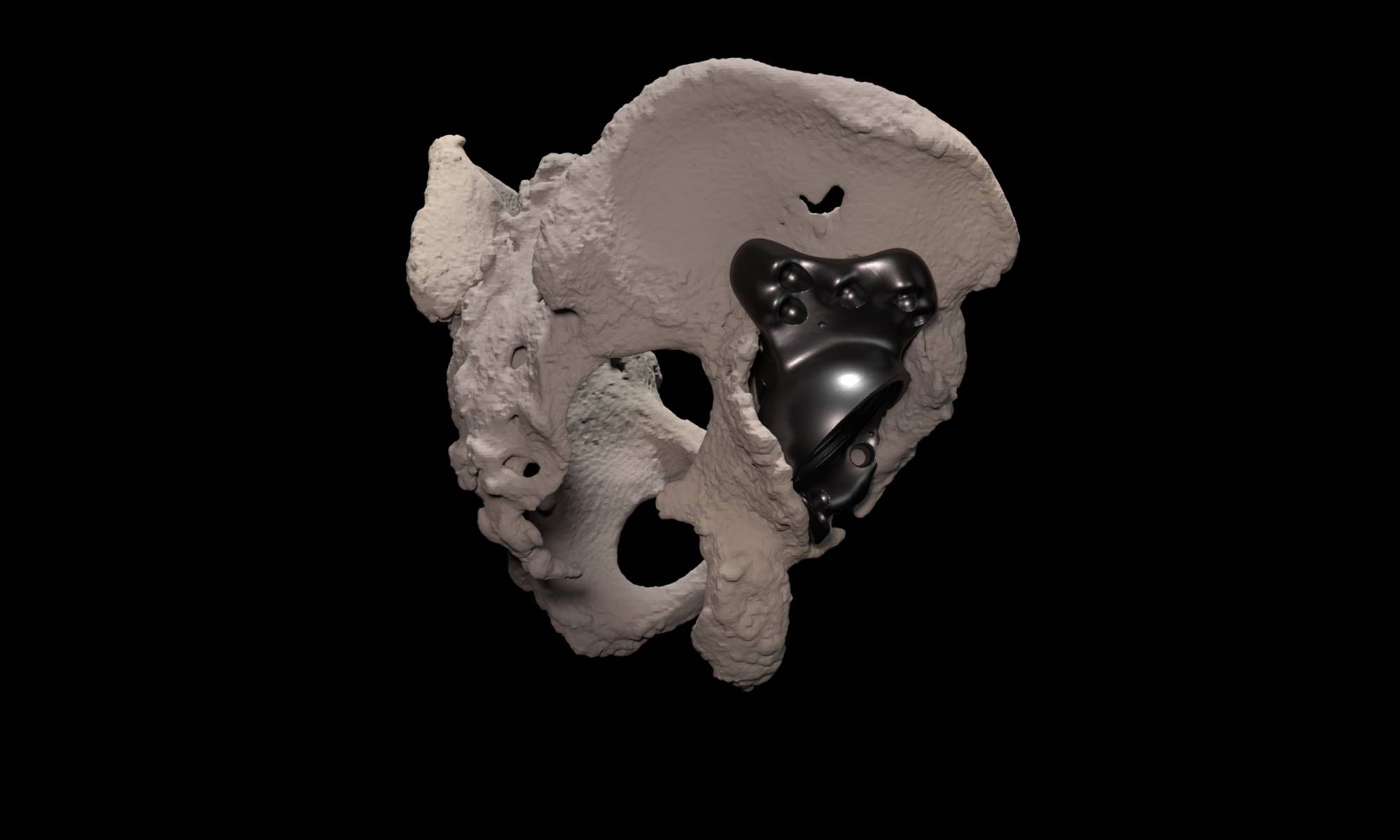
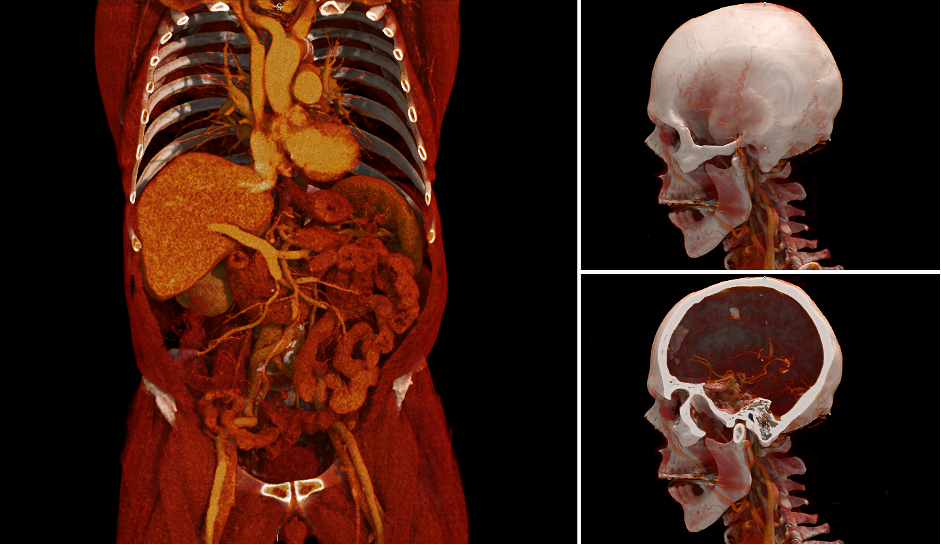
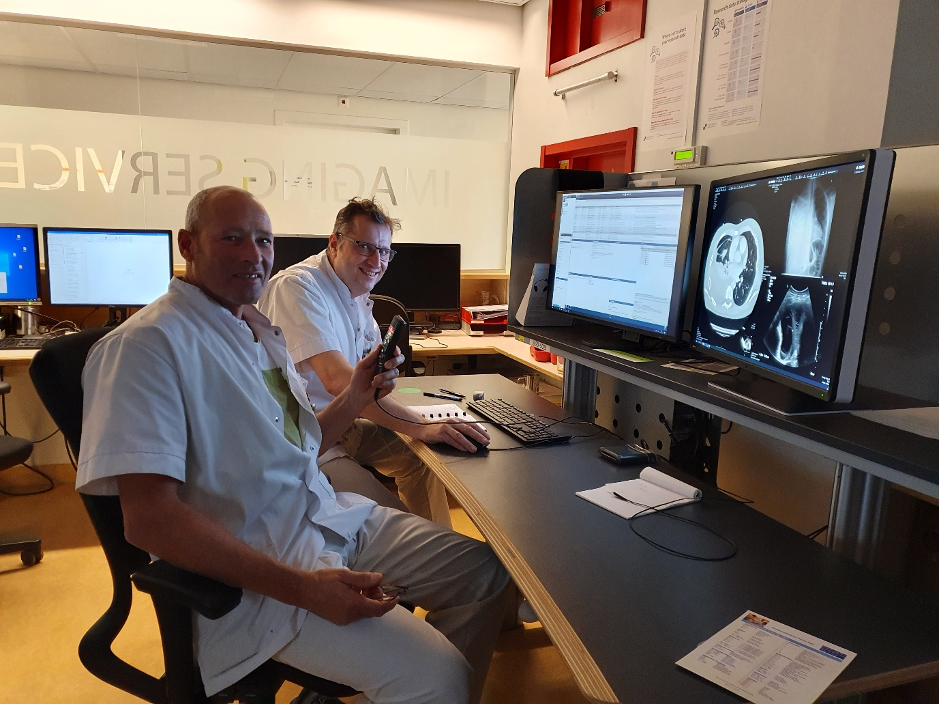
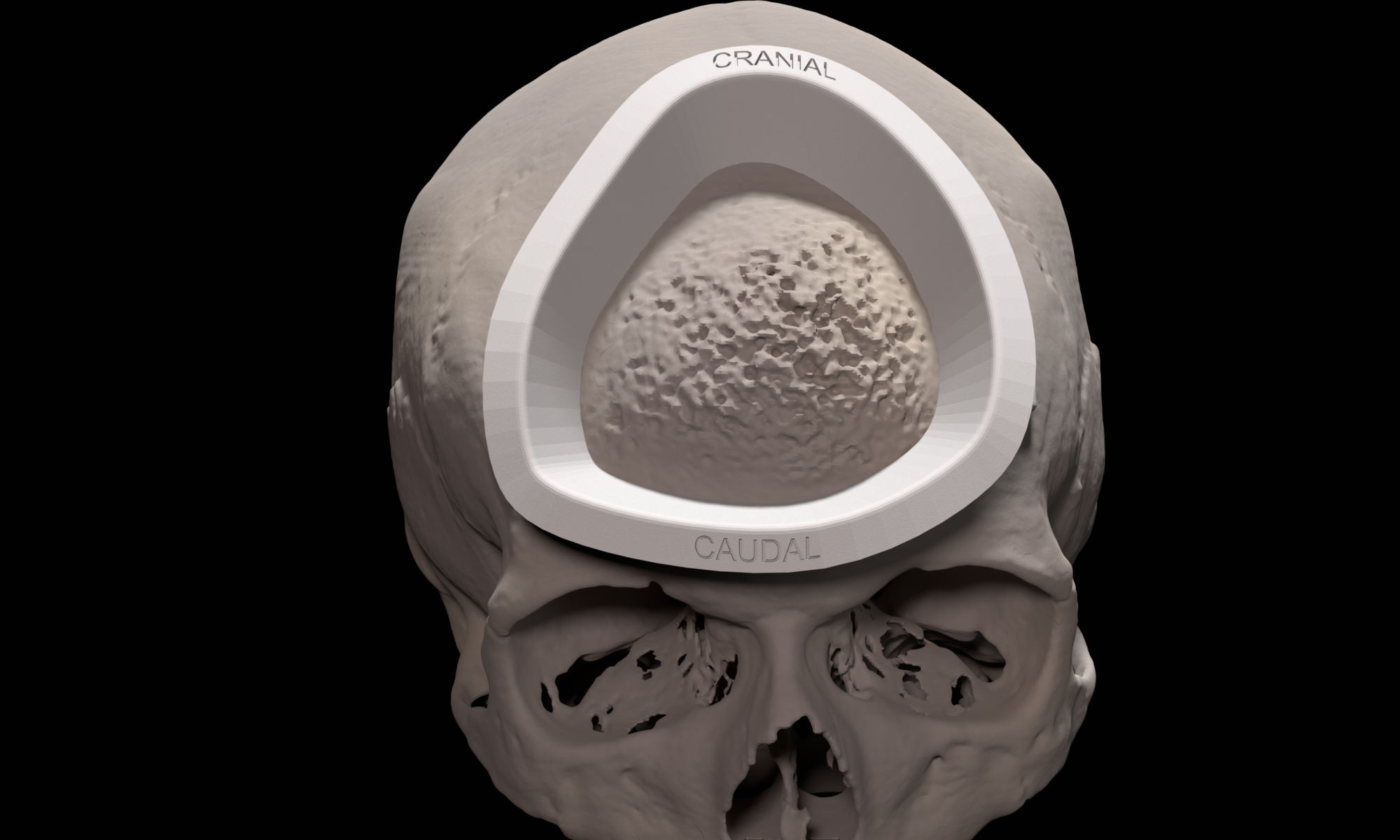
Custom designed 3D printed implants offer a solution in patients where other reconstruction options are not available. For the design and fabrication of these implants, we collaborate with different companies.
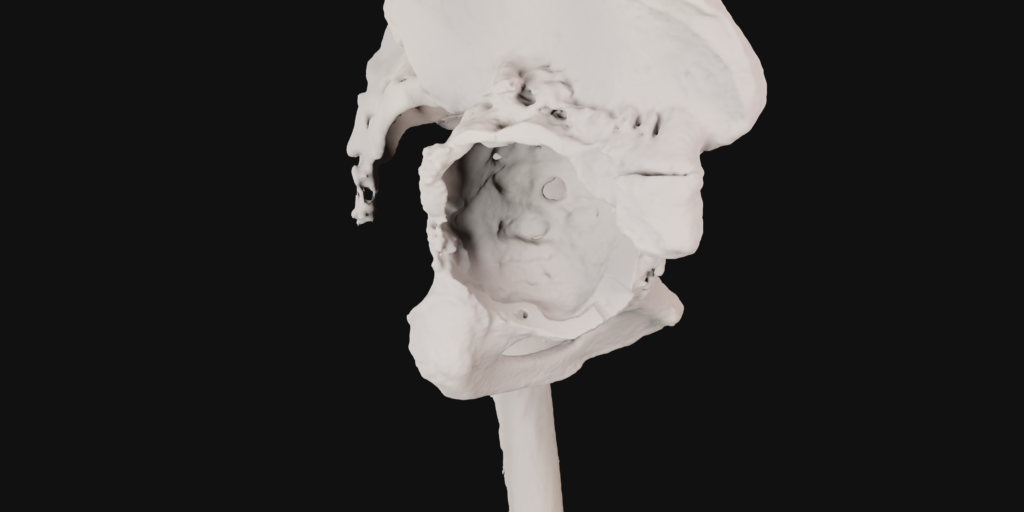
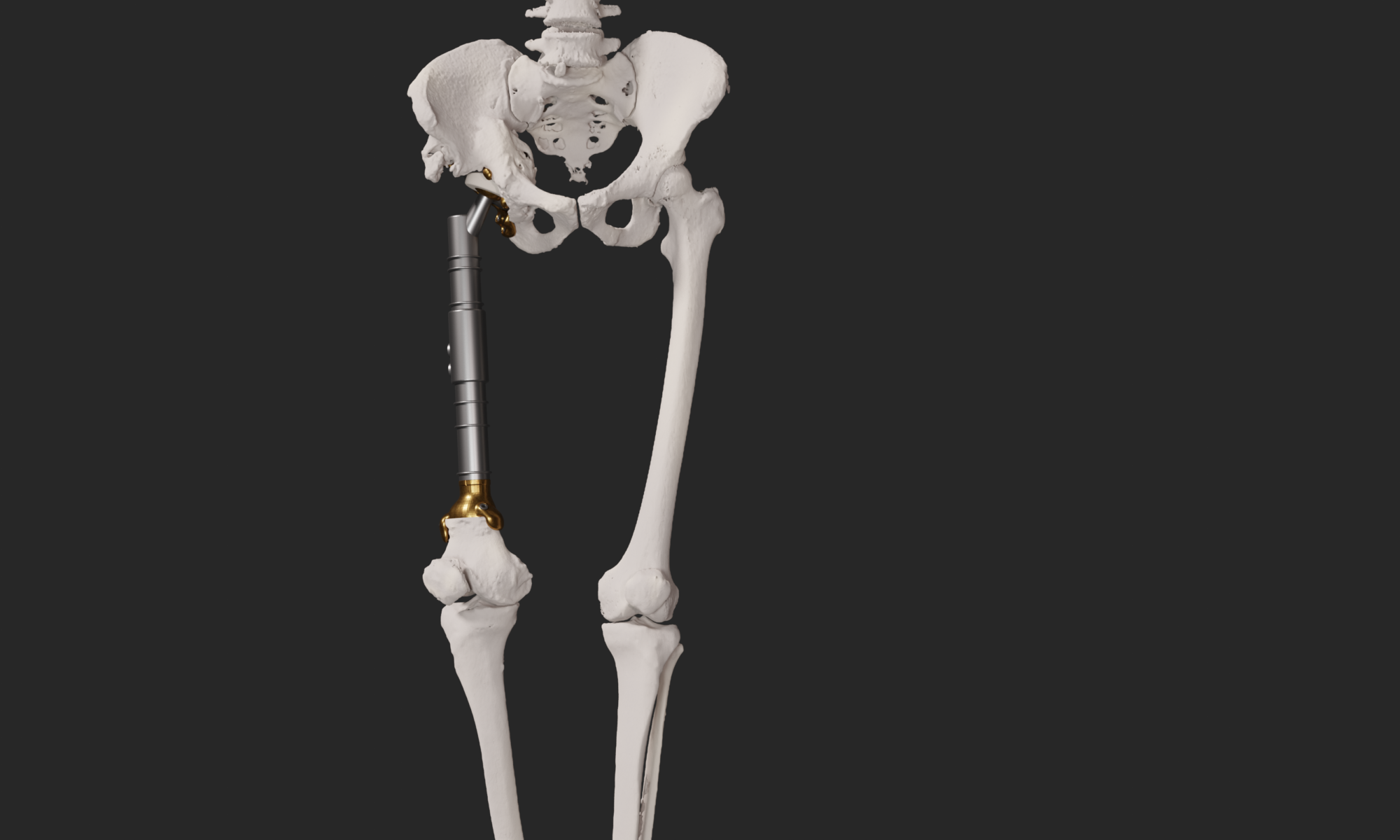
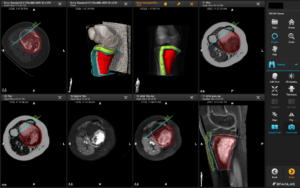
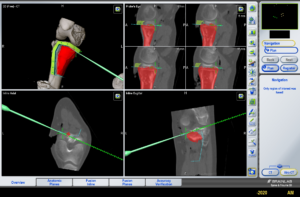
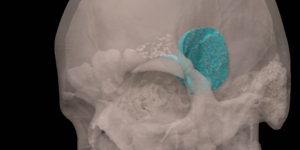
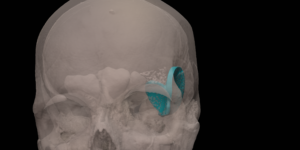
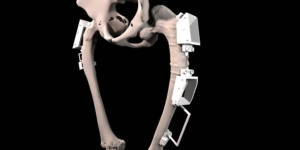
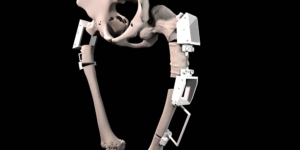
A 41 year old female suffered a combination of a large acetabular and a subtotal femoral defect, due to a chronic low grade periprosthetic joint infection of a revision total hip replacement.
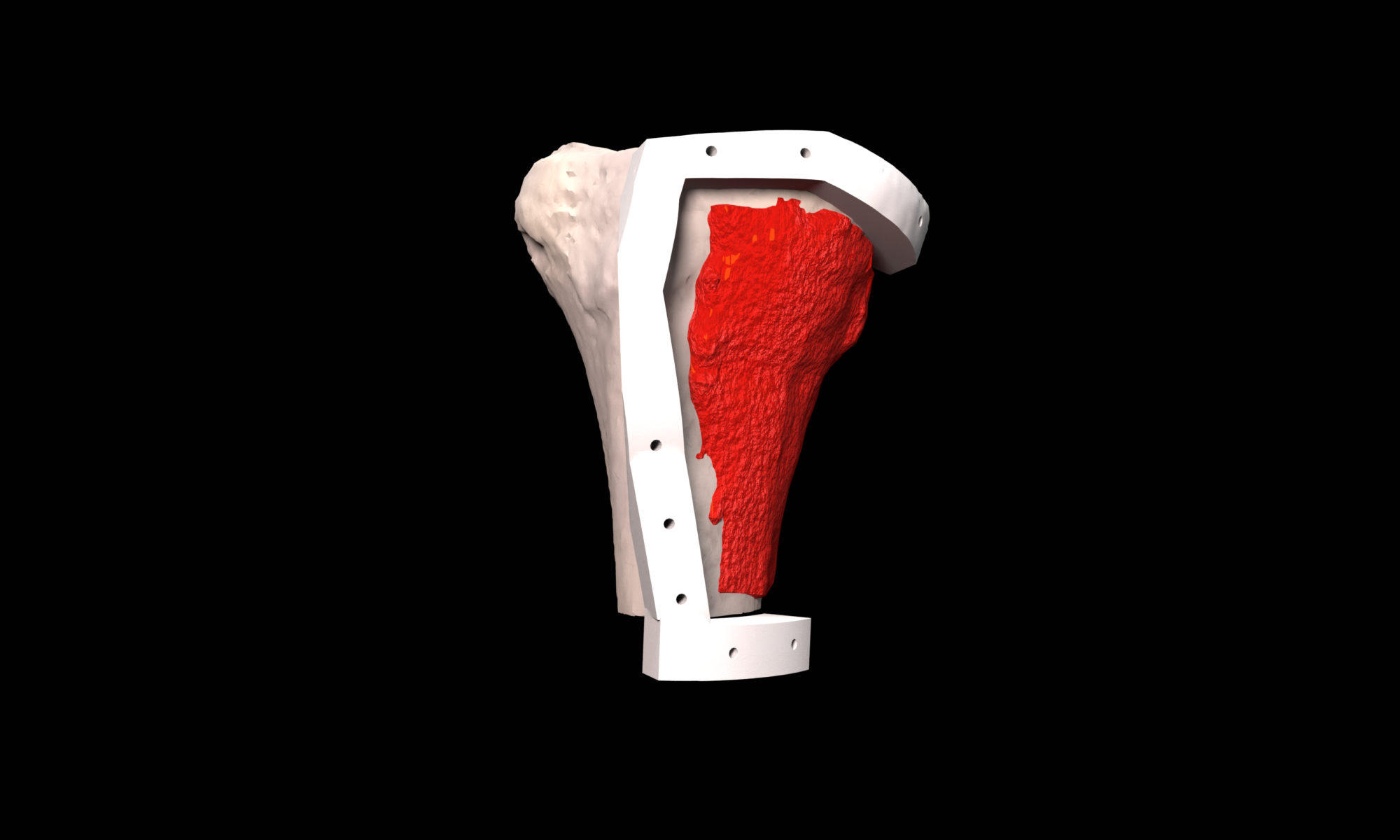
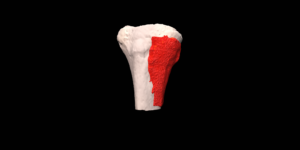
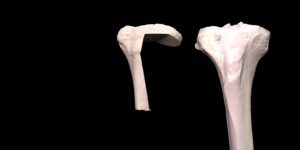
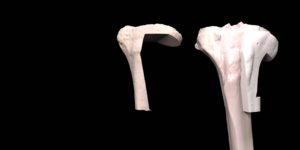
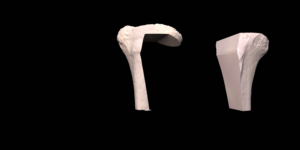
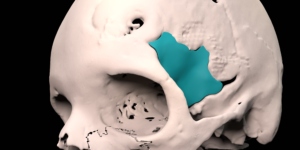
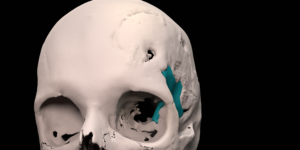
The final procedure included reconstruction of the pelvis with an OSSIS® AceOs plus custom acetabular implant. Femoral reconstruction was performed using a MUTARS® proximal femoral replacement with a custom MUTARS C-fit 3D printed joint sparing fixation, preserving the native knee joint and with this preventing the necessity for total femoral replacement.